Blogs
How to Detect PCOS
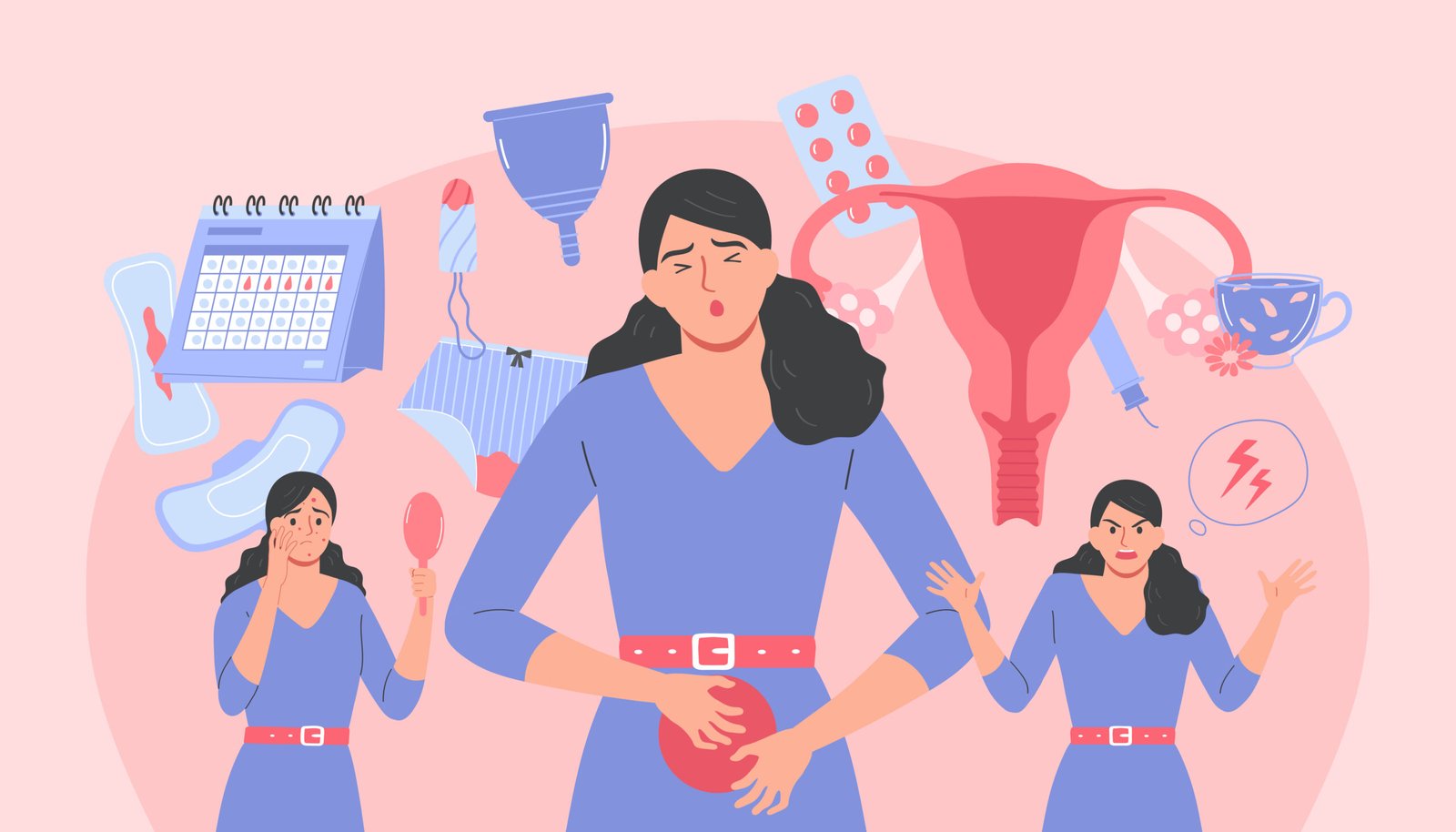
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects many women of reproductive age. Early detection is crucial for managing the condition effectively and preventing long-term health complications. This blog will guide you through the symptoms, diagnosis process, and what to do if you suspect you have PCOS.
Understanding PCOS
PCOS is characterized by hormonal imbalances that can lead to a variety of symptoms. It’s important to recognize these signs early to seek appropriate medical advice and treatment.
Common Symptoms of PCOS
The symptoms of PCOS can vary from person to person, but some common signs include:
1. Irregular Periods
One of the most common indicators of PCOS is irregular menstrual cycles. This could mean periods that are infrequent, prolonged, or completely absent.
2. Excessive Hair Growth
Known as hirsutism, excessive hair growth on the face, chest, back, or other areas can be a result of elevated androgen levels.
3. Acne and Oily Skin
Hormonal imbalances can lead to persistent acne and excessively oily skin, particularly around the face, chest, and upper back.
4. Weight Gain
Many women with PCOS experience unexplained weight gain or difficulty losing weight, often concentrated around the abdomen.
5. Thinning Hair or Hair Loss
PCOS can cause hair thinning or hair loss, similar to male-pattern baldness, due to elevated androgen levels.
6. Fertility Issues
PCOS is one of the leading causes of infertility in women due to irregular ovulation or anovulation (absence of ovulation).
How is PCOS Diagnosed?
Diagnosing PCOS involves a combination of medical history, physical examination, and diagnostic tests. Here’s what you can expect:
1. Medical History
Your doctor will ask about your menstrual cycle, weight changes, and any other symptoms you may have noticed. They may also inquire about your family history, as PCOS can run in families.
2. Physical Examination
A physical exam may include checking for signs of hirsutism, acne, and other physical indicators of hormonal imbalance.
3. Blood Tests
Blood tests can measure hormone levels, including androgen, insulin, and glucose levels, to help identify hormonal imbalances associated with PCOS.
4. Ultrasound
An ultrasound may be performed to check for the presence of multiple cysts on the ovaries and assess the thickness of the uterine lining. This helps confirm the diagnosis of PCOS.
Next Steps After Diagnosis
If you are diagnosed with PCOS, it’s important to work closely with your healthcare provider to manage the condition. Here are some common management strategies:
1. Lifestyle Changes
Adopting a healthier lifestyle through a balanced diet, regular exercise, and weight management can help regulate your menstrual cycle and reduce symptoms.
2. Medications
Depending on your symptoms and goals, your doctor may prescribe medications such as birth control pills to regulate periods, anti-androgens to reduce excessive hair growth, or insulin-sensitizing drugs like metformin.
3. Fertility Treatments
If you’re trying to conceive, fertility treatments such as ovulation-inducing medications or assisted reproductive technologies may be recommended.
4. Managing Other Health Risks
PCOS is associated with an increased risk of developing type 2 diabetes, cardiovascular disease, and endometrial cancer. Regular check-ups and proactive management of these risks are essential.
For those seeking natural support in managing PCOS symptoms, our product, PCOS Wellness, offers a holistic approach. Designed to aid hormonal balance, improve menstrual regularity, and alleviate common symptoms, PCOS Wellness can be an integral part of your journey toward better health and well-being.
